Sessions & Tracks
Cancer Cell Biology & Genetics
Cancer cell biology focuses on the structure and function of cancer cells. Cancer is characterized by abnormal cell growth, with the potential to invade or spread to other parts of the body, distinguishing it from benign tumors. Normal cell division aids growth and repair, but cancer cells persistently divide, ignoring the body's signals to stop. This unregulated growth often leads to metastasis, where cancer spreads to other parts of the body. Genetic mutations causing DNA damage and genomic instability are primary drivers of cancer formation.
Cancer & Stem Cell Therapy
Cancer stem cells (CSCs) exhibit traits similar to normal stem cells, including self-renewal and differentiation. CSCs are tumorigenic and may resist conventional chemotherapeutic agents. Their unique properties, such as enhanced DNA repair and resistance mechanisms, make them difficult to eliminate. Developing targeted therapies for CSCs offers hope for improving survival rates and quality of life for patients with metastatic cancer.
Cancer Biomarkers
Biomarkers are molecules that indicate the presence of cancer, either through tumor-derived substances or bodily responses to tumors. Biomarkers assist in cancer diagnosis, prognosis, and monitoring. Examples include AFP (liver cancer), BCR-ABL (chronic myeloid leukemia), and BRCA1/BRCA2 (breast/ovarian cancer). Non-invasive biomarker testing using blood or bodily fluids holds promise for early detection.
Breast Cancer
Breast cancer is one of the most common cancers worldwide, affecting both women and, less frequently, men. It occurs when abnormal cells in the breast grow uncontrollably, forming a tumor that may spread to other parts of the body. The main types include ductal carcinoma and lobular carcinoma. Risk factors include genetics, hormonal changes, obesity, and lifestyle choices. Symptoms may include a lump in the breast, changes in breast shape, nipple discharge, or skin dimpling. Early detection through mammograms and self-examinations improves survival rates. Treatment options include surgery, chemotherapy, radiation therapy, hormone therapy, and targeted therapies.
Hematologic Malignancies
Hematologic malignancies are cancers that affect the blood, bone marrow, and lymphatic system. They include leukemia, lymphoma, and myeloma. Leukemia involves abnormal white blood cells, while lymphoma affects the lymph nodes and immune system. Myeloma is cancer of the plasma cells in the bone marrow. Risk factors include genetic predisposition, environmental exposures, and certain viral infections. Symptoms may include fatigue, frequent infections, unexplained weight loss, and swollen lymph nodes. Treatment often involves chemotherapy, radiation therapy, stem cell transplantation, targeted therapies, and immunotherapy, with advances in precision medicine improving outcomes for many patients. Early diagnosis is crucial for effective treatment.
Radiation Oncology
Radiation oncology is a medical specialty focused on using radiation therapy to treat cancer and certain non-cancerous conditions. It involves the precise delivery of high-energy radiation to destroy cancer cells while minimizing damage to healthy tissues. Common types of radiation therapy include external beam radiation therapy (EBRT) and brachytherapy. Radiation oncology plays a crucial role in cancer treatment, either as a primary therapy or in combination with surgery, chemotherapy, or immunotherapy. Advanced techniques like IMRT, proton therapy, and stereotactic radiosurgery improve treatment accuracy and patient outcomes. Side effects vary but may include fatigue, skin irritation, and localized pain.
Gynecologic Oncology
Gynecologic oncology is a specialized field of medicine focused on the prevention, diagnosis, and treatment of cancers affecting the female reproductive system. These include ovarian, cervical, uterine, vaginal, and vulvar cancers. Risk factors vary but may include HPV infection, genetic mutations (e.g., BRCA genes), hormonal influences, and lifestyle factors. Early symptoms can be subtle, such as abnormal bleeding, pelvic pain, bloating, or unexplained weight loss. Treatment options include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Regular screenings, such as Pap smears and HPV testing, play a key role in early detection and improving survival rates.
Gastrointestinal Cancers
Gastrointestinal (GI) cancers affect the digestive tract, including the esophagus, stomach, liver, pancreas, colorectal, and rectum. Risk factors include diet, family history, smoking, and certain genetic conditions. Symptoms vary but may include abdominal pain, changes in bowel habits, weight loss, and difficulty swallowing. Early detection and screening (e.g., colonoscopy) are critical. Treatment options include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy, depending on the cancer type and stage.
Genitourinary Cancers
Genitourinary cancers affect the kidneys, bladder, prostate, testicles, and ureters. These cancers are more common in men, particularly prostate cancer. Smoking, family history, age, and exposure to certain chemicals are known risk factors. Symptoms may include blood in urine, pelvic pain, urinary changes, or unexplained weight loss. Treatment often involves surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Early detection, such as regular prostate screenings or kidney function tests, improves treatment outcomes.
Pediatric Hematology/Oncology
Pediatric hematology/oncology focuses on diagnosing and treating blood disorders and cancers in children. Common conditions include leukemia, lymphoma, and solid tumors. Childhood cancers often present with pale skin, unusual bruising, fatigue, or unexplained lumps. Treatment varies but typically includes chemotherapy, radiation, stem cell transplantation, and targeted therapies. Early detection and ongoing research have significantly improved survival rates for many childhood cancers. Supportive care, including pain management and psychological support, is integral to treatment.
Cancer Biomarkers
Biomarkers are molecules that indicate the presence of cancer, either through tumor-derived substances or bodily responses to tumors. Biomarkers assist in cancer diagnosis, prognosis, and monitoring. Examples include AFP (liver cancer), BCR-ABL (chronic myeloid leukemia), and BRCA1/BRCA2 (breast/ovarian cancer). Non-invasive biomarker testing using blood or bodily fluids holds promise for early detection.
Cancer Screening & Chemotherapy
Screening aims to detect cancer early, improving treatment outcomes. Reliable methods such as blood tests, imaging, and DNA analysis are essential. Chemotherapy, a cornerstone of cancer treatment, involves anti-cancer drugs to eliminate or slow tumor growth. It can be curative or palliative, often used in combination with other therapies to enhance effectiveness.
Cancer Causes and Risk Factors
Cancer arises from genetic mutations leading to uncontrolled cell growth. Environmental and lifestyle factors, such as smoking, poor diet, obesity, infections, and radiation exposure, play significant roles. Hormonal imbalances, chronic inflammation, and viral infections are additional contributors. Awareness of these factors is critical for prevention and early intervention.
Cancer Early Detection, Diagnosis, and Prognosis
Early detection of cancer through symptoms, screening, and diagnostic tests like imaging and biopsies is crucial for better outcomes. Prognosis refers to predicting disease progression, which guides treatment decisions and provides insight into expected quality of life.
Cancer Awareness and Survival
Raising awareness about cancer symptoms and risk factors can significantly improve survival rates. Socioeconomic disparities often affect access to quality care. Campaigns and educational programs must focus on underserved populations to enhance early diagnosis and treatment adherence.
Cancer Prevention & Research
Preventative measures such as avoiding tobacco, maintaining a healthy weight, and staying physically active can reduce cancer risk. Advances in cancer research focus on understanding its causes, developing treatments, and exploring preventive vaccines.
Tumor Virology, Immunology & Cellular Pathology
Certain viruses, such as HPV and Hepatitis B, are associated with cancer development. Cancer immunology studies the immune system's role in combating tumors, paving the way for immunotherapies that activate the body’s defenses to target cancer cells.
Cancer Biopsy
Biopsies are essential for diagnosing cancer, involving the examination of tissue samples under a microscope. They provide critical insights into tumor type, stage, and genetic profile, guiding personalized treatment approaches.
Surgical and Clinical Oncology
Surgical oncology involves removing tumors through advanced techniques like laparoscopic and robotic surgery, ensuring precision and minimal recovery time. Clinical oncologists use chemotherapy, radiotherapy, and systemic treatments to manage cancer, working in multidisciplinary teams to tailor care.
Market Analysis
Cancer Medicine, Radiology & Treatment Market Analysis (Up to 2026)
The global cancer medicine, radiology, and treatment market continues to expand rapidly, driven by rising cancer prevalence, technological advancements, and heavy investment in R&D. By 2026, the oncology market is expected to surpass USD 500 billion, fueled by growth in therapeutics, diagnostics, and advanced imaging systems. Therapeutics remain the largest segment, supported by increased adoption of immunotherapies, targeted therapies, and precision medicine. The radiology sector—including CT, MRI, PET, and interventional imaging—is projected to grow steadily at 6–8% CAGR, driven by AI-powered diagnostics, early detection tools, and minimally invasive imaging-guided therapies.
Key regions:
-
North America: Continues to lead due to innovation and strong healthcare infrastructure.
-
Asia-Pacific: Fastest-growing, with expanding healthcare access in India and China.
Growth drivers:
-
Increasing cancer cases (19M+ annually)
-
AI integration for radiology and treatment planning
-
Liquid biopsies, proton therapy, nanomedicine, and genomic profiling
-
Government support for screening and early detection
Challenges: High treatment costs, regulatory delays, and therapy resistance.
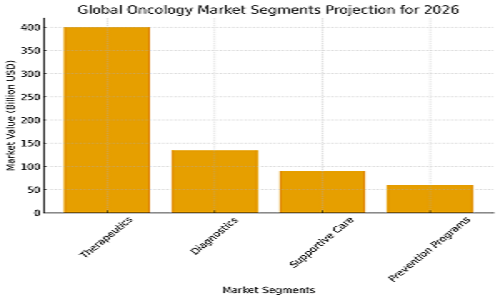
2026 Oncology Market Snapshot (Global Segments)
Projected Market Share 2026:
-
Therapeutics: ~400+ billion USD
-
Diagnostics: ~135 billion USD
-
Supportive Care: ~90 billion USD
-
Prevention Programs: ~60 billion USD
This reflects continued dominance of therapeutics and strong growth in diagnostics and supportive innovation.
If you want, I can convert this into a graph, brochure paragraph, or conference report format.
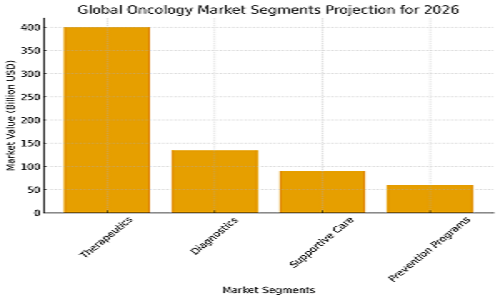
Here bar graph representing the global oncology market segmentation projection for 2026.